Services
Hip Osteoarthritis
Overview
Hip osteoarthritis is a degenerative disease involving the cartilage in the hip joint. Osteoarthritis occurs when the protective cartilage surrounding the end of your bone begins to wear down over time. It can most commonly affect the knees, hips, hands, and spine. Symptoms can usually be managed but the damage to the joints can never be reversed.
Risk factors for developing osteoarthritis include age, gender, obesity, previous joint injuries, repetitive stress on a joint, genetics, bone deformities, and metabolic disorders.
Symptoms
Symptoms of osteoarthritis develop slowly over time and can vary from person to person. Most commonly, patients will experience joint pain, stiffness (especially in the morning), tenderness around the joint, loss of flexibility or range of motion, grating sensation, and swelling.
Diagnosis
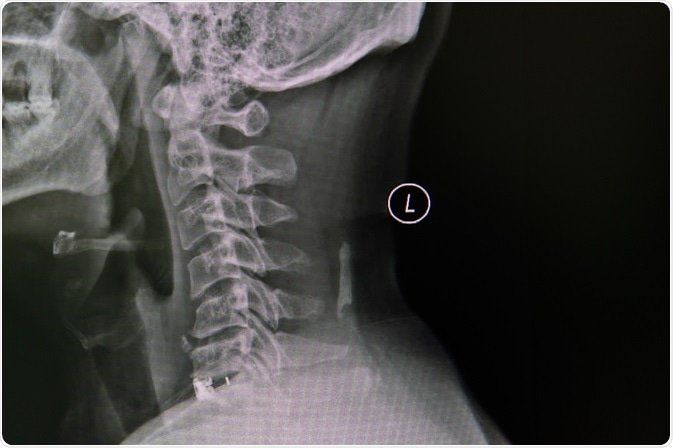
Diagnosis of osteoarthritis of a joint can be made with x-ray of the joint. MRI may also be useful in diagnosing osteoarthritis.
Treatment
Treatment of osteoarthritis first begins with lifestyle changes including consistent exercise and proper weight management.
Physical therapy and pool therapy have also been shown to be effective in helping treat
osteoarthritis pain. Additionally, alternative movement therapies such as tai-chi and yoga have been found to help reduce pain caused by osteoarthritis.
Traditional medication options include acetaminophen (tylenol), and non-steroidal anti-
inflammatory drugs (NSAIDs) such as ibuprofen, or aleve.
Supplements such as glucosamine/chondroitin, capsaicin, and omega-3 fatty acids, while controversial in efficacy, have anecdotally reduced patient’s osteoarthritis pain.
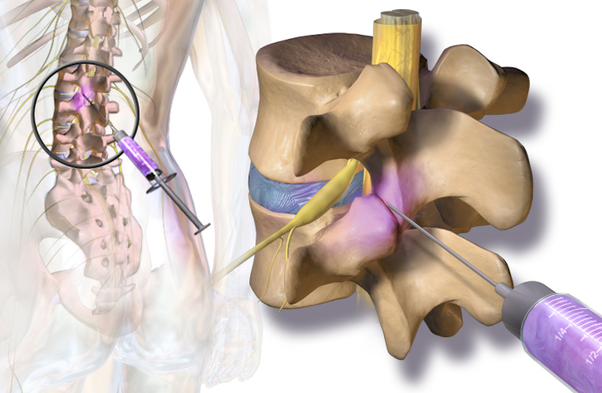
Typically, if lifestyle changes, therapies, and medications fail to relieve pain, then cortisone or steroid injections can be performed to help reduce inflammation in the hip joint.
Finally, if all conservative measures fail the patient can undergo surgery to replace the hip joint. This is typically done by an orthopedic surgeon.