Diagnosing Fibromyalgia
Fibromyalgia is a condition which in the past has been a diagnosis of exclusion. This meant that a person was only diagnosed with the condition after all other possible causes of pain were ruled out. In the 1990’s, the American College of Rheumatology (ACR) made the diagnosis of fibromyalgia more clear cut. The ACR’s definition involved assessing an individual who has widespread chronic pain for tender points. 18 specific tender points in the body were described by the ACR. If an individual had 13 out of 18 tender points, then they would meet the criteria for fibromyalgia.
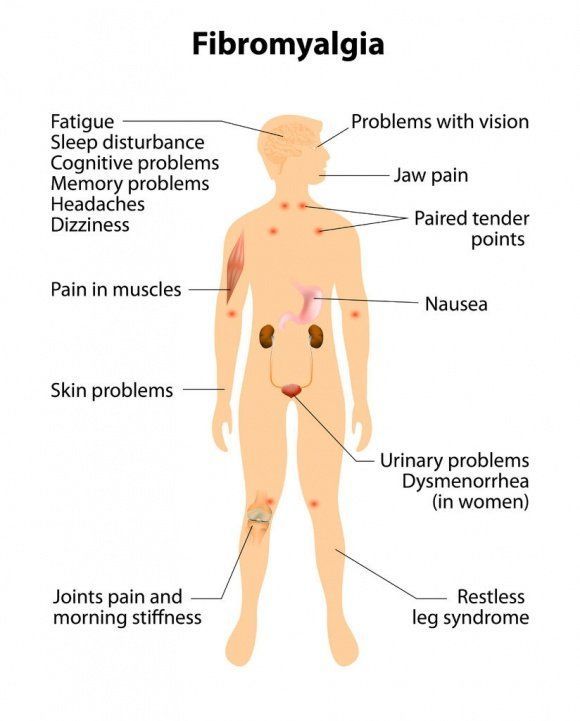
Recently the diagnosis of fibromyalgia has been streamlined. The tender point identification is not essential and fibromyalgia is no longer a diagnosis of exclusion. The modern definition requires that a patient have chronic widespread pain that is present for more than 3-6 months. The pain should be symmetric. It should be on the right side of the body, as well as the left side of the body. The pain should be present above the waist and below the waist. It should be present along the spine and in the limbs. The pain of fibromyalgia will typically be associated with muscle stiffness, sleep disturbance and may be associated with irritable bowel syndrome.
The above definition of fibromyagia is the most practical way to make an accurate diagnosis. There are other ways to confirm the diagnosis. Brain scans called functional magnetic resonance imaging studies (fMRIs) have shown increased activity in pain centers in the brain in patients with fibromyalgia. Researchers have also shown increased levels of pain neurotransmitters in the cerebral spinal fluid of patient with fibromyalgia.
If you have symptoms of chronic widespread pain with morning stiffness and sleep disorder that has lasted for more than 3-6 months, you should discuss your symptoms with your health care providers. There are now FDA approved medication therapy to treat and manage fibromyalgia.