November 7, 2024
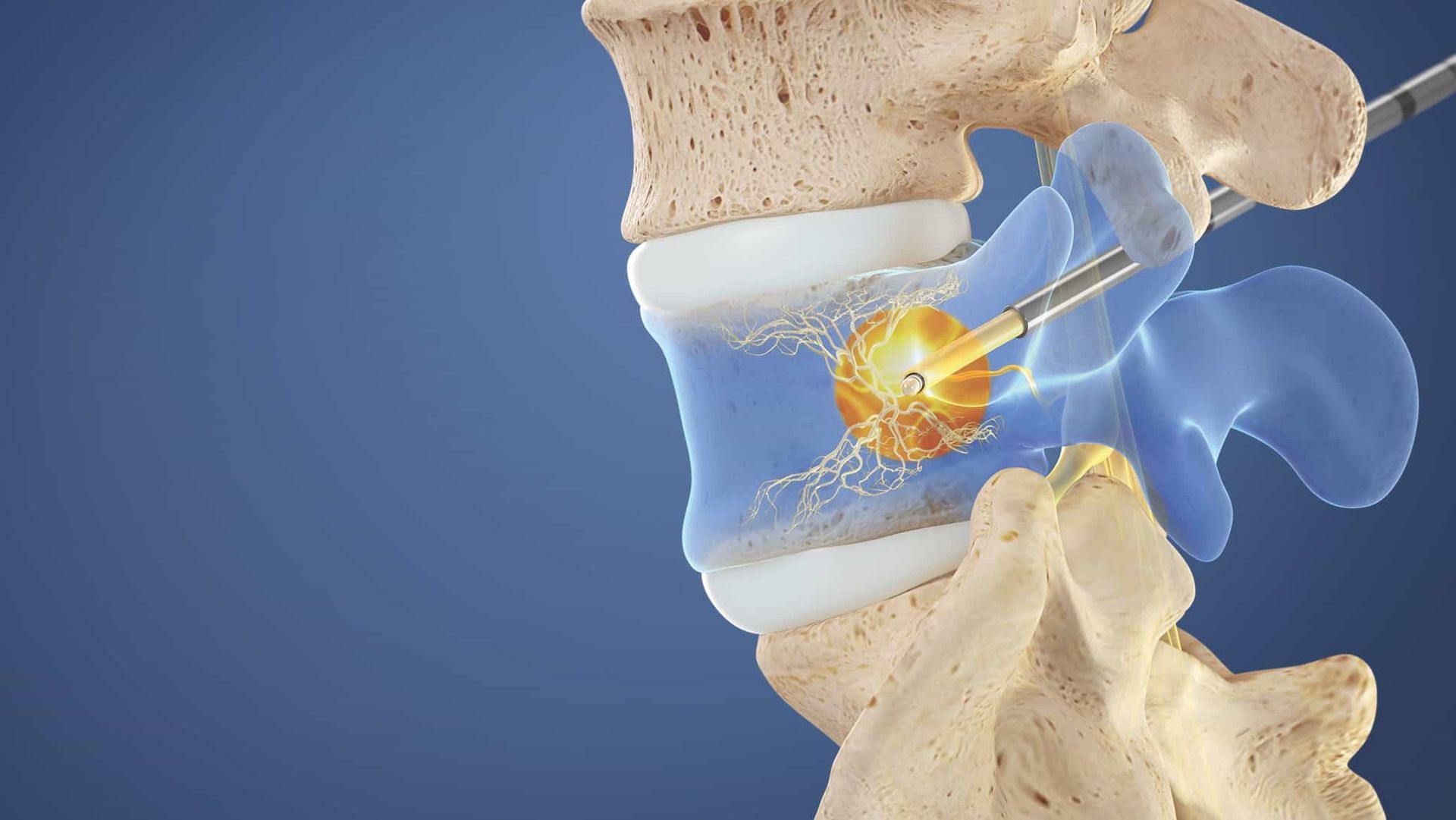
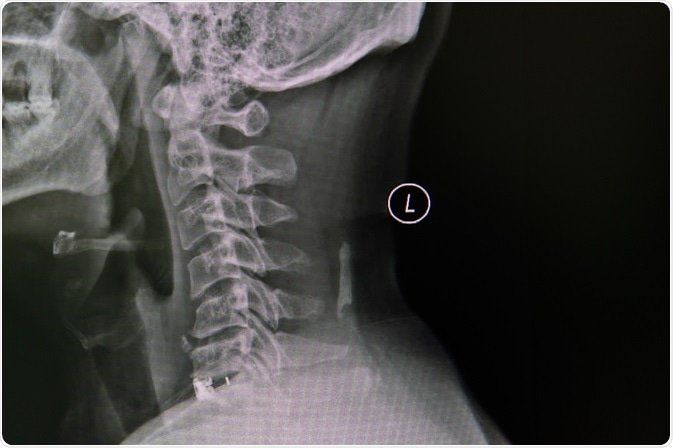
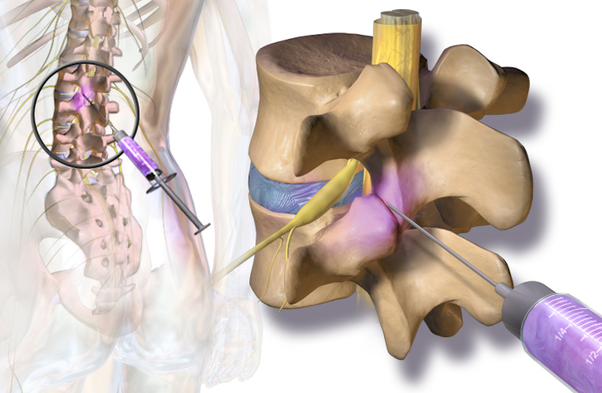
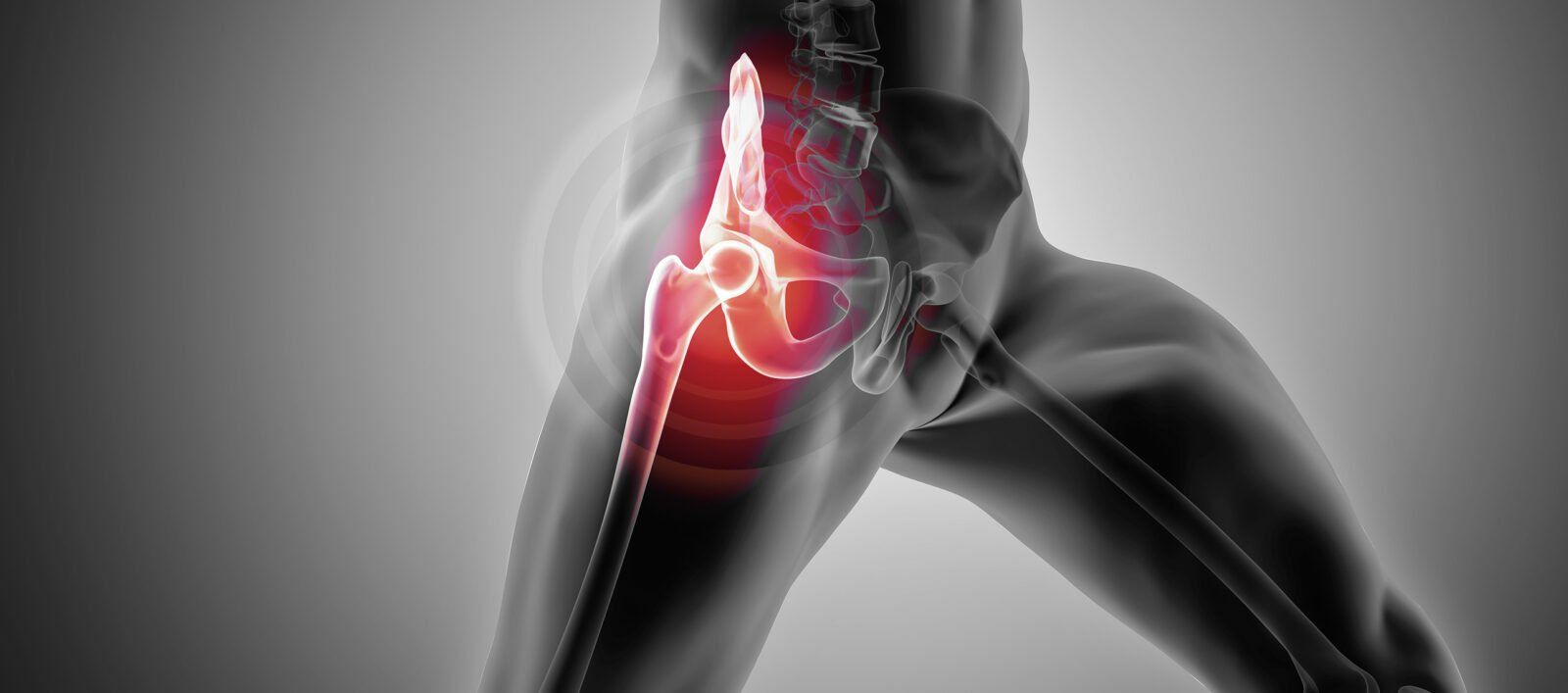
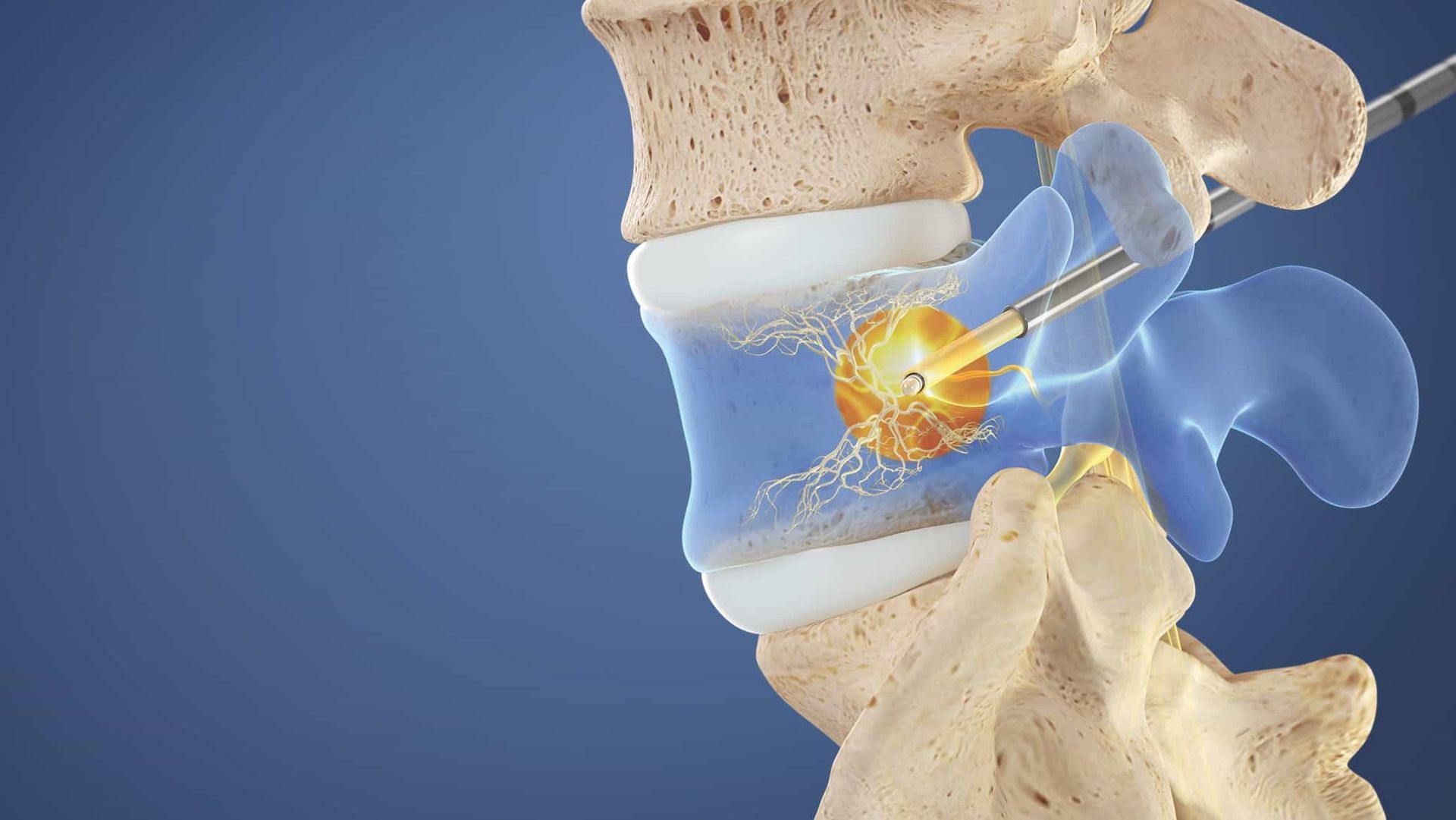
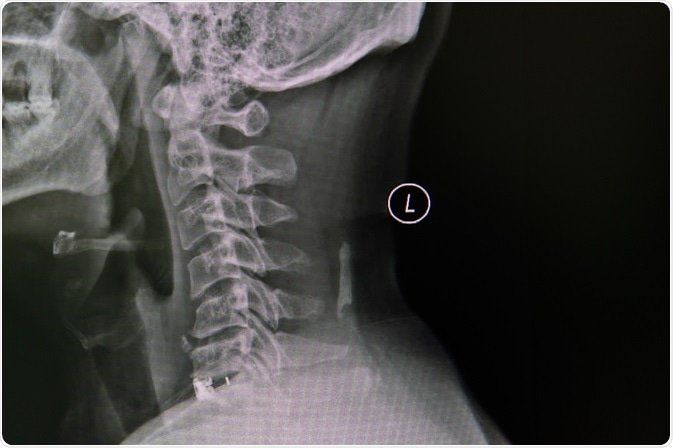
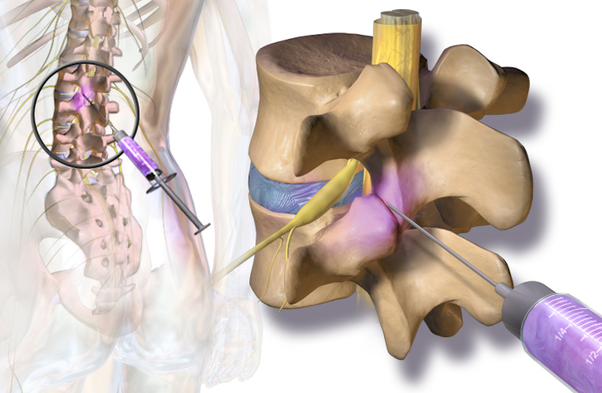
Understanding Basivertebral Nerve Ablation (Intracept) for Chronic Low Back Pain Chronic low back pain is one of the most common complaints among patients, affecting quality of life, mobility, and even mental well-being. While there are many causes of low back pain, one source that's often overlooked is vertebrogenic pain—pain originating from the vertebral endplates. Basivertebral nerve ablation, also known as the Intracept procedure, is an innovative, minimally invasive treatment specifically designed to target this type of pain at its source. What is Vertebrogenic Pain? Vertebrogenic pain occurs when the vertebral endplates—where the vertebrae connect to the spinal discs—become damaged or inflamed. This can lead to chronic pain that’s resistant to traditional therapies like physical therapy, medications, and even other types of spinal injections. For years, there weren't many effective treatments for vertebrogenic pain. But recent advancements in medical technology have led to the development of the Intracept procedure. What is the Intracept Procedure? The Intracept procedure is a minimally invasive treatment that targets the basivertebral nerve, which transmits pain signals from the vertebral endplates. By ablating, or "turning off," this nerve, the Intracept procedure disrupts the pain pathway, providing significant and lasting relief for many patients. How Does It Work? During the procedure, a specialized probe is inserted into the vertebra through a small incision. Using radiofrequency energy, the probe heats and ablates the basivertebral nerve, effectively "shutting down" the pain signal being sent from the damaged vertebra. The entire procedure typically takes about an hour and is performed on an outpatient basis, meaning most patients can go home the same day. Who is a Candidate? The Intracept procedure is intended for patients who: Have been experiencing chronic low back pain for more than six months. Have not found relief from conservative treatments like physical therapy, medications, or injections. Have MRI findings that indicate Modic changes, a marker of inflammation and degeneration in the vertebral endplates. Do not have significant disc or nerve compression that would otherwise explain their pain. Benefits of Basivertebral Nerve Ablation Long-Lasting Pain Relief : Many patients experience significant pain reduction that lasts years after the procedure . Minimally Invasive : This outpatient procedure requires only a small incision, leading to quicker recovery times compared to traditional back surgeries. Improved Quality of Life : By targeting the nerve responsible for vertebrogenic pain, the Intracept procedure can restore function and improve quality of life. What to Expect After the Procedure Recovery time varies, but most patients can return to normal activities within a few days. You may experience some soreness at the treatment site, but this typically resolves quickly. Patients often report gradual improvement in their pain levels over several weeks, with the best results seen at the 3- to 6-month mark. Is Intracept Right for You? If you’ve been dealing with chronic low back pain that hasn’t responded to other treatments, and if MRI findings suggest Modic changes in your vertebrae, the Intracept procedure may be worth considering. It’s important to consult with a specialist who can evaluate your unique situation and help determine if basivertebral nerve ablation is the right option for you. Final Thoughts At Spine & Nerve, we’re committed to providing innovative, evidence-based treatments to help our patients find relief and improve their quality of life. The Intracept procedure is a promising solution for those suffering from vertebrogenic pain, offering an option where traditional therapies may fall short. If you’re ready to explore whether basivertebral nerve ablation could be the answer to your chronic low back pain, reach out to our team to schedule a consultation. Together, we’ll work to find the best treatment plan to get you back to living your life, pain-free.